Coming into contact with aversive internal experiences—thoughts, emotions, sensations—is an essential part of healing through therapy. Therapists work with clients to raise awareness of experiential avoidance and disengage costly control strategies. This is accomplished via exercises targeting openness to internal experiences. When conducting therapy via telehealth, therapists may find their repertoire of experiential exercises becomes truncated by remoteness, technological limitations, or access to resources. On the other end of the line, these same factors may enable or exacerbate experiential avoidance in our clients.
Therapists should be both flexible and steadfast when conducting therapy remotely. We must remain committed to therapeutic processes that work, while adapting our procedures to new circumstances. However, like our clients, we have minds that may seek to allay anxiety, frustration, or self-consciousness related to this new context for therapy in unworkable ways. Rather than collude with a control agenda that may exploit the disconnect imposed by telehealth as a means of avoidance, therapists should model openness to experience and remain committed to high-quality, process-based care.
Several practical strategies may help therapists navigate the shift to remote therapy or enhance their telehealth practice. First, be proactive. Review your repertoire of tools and techniques for engaging therapeutic processes. Identify which would be difficult or impossible via video or phone. Then, make adaptations. Second, be intentional. Encourage your clients (and yourself) to dedicate time, space, and energy to the therapy. Clients ought not complete sessions while engaged in other tasks (e.g., work, childcare). Therapists, rather than engaging urges to multitask, should work to deepen the connection to the patient. Finally, be compassionate. Glitches, freezes, and dropped calls can short-circuit some of the observational skills we have honed as therapists. Our attention skills are stretched in different ways. If you notice frustration, agitation, or exhaustion, do so mindfully and with self-kindness. Our common humanity connects us, even from afar.
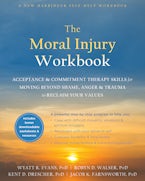
Wyatt R. Evans, PhD, is a board-certified clinical psychologist with the VA North Texas Health Care System, and therapist in private practice in the Dallas-Fort Worth area. His primary areas of expertise are resilience and post-traumatic stress, including moral injury. He is committed to advancing interventions, especially acceptance and commitment therapy (ACT), to promote recovery and enhance resilience for service members, veterans, and others highly affected by trauma.


 Why Journaling Is Especially Helpful to Adult Children of Emotionally Immature Parents
Why Journaling Is Especially Helpful to Adult Children of Emotionally Immature Parents